Clinical Studies – Targeting Acute and Chronic Thromboembolic Disorders
Prevention of Bleeding in Patients with Atrial Fibrillation Undergoing PCI with Stenting
PIONEER AF-PCI:
An Open-Label, Randomised, Controlled, Multicentre Study Exploring Two Treatment Strategies of Rivaroxaban and a Dose-Adjusted Oral VKA Treatment Strategy in Subjects with AF who Undergo PCI
Objective
- To compare the safety of the following three treatment strategies after PCI with stent placement in patients with paroxysmal, persistent, or permanent non-valvular atrial fibrillation1
Study Design1
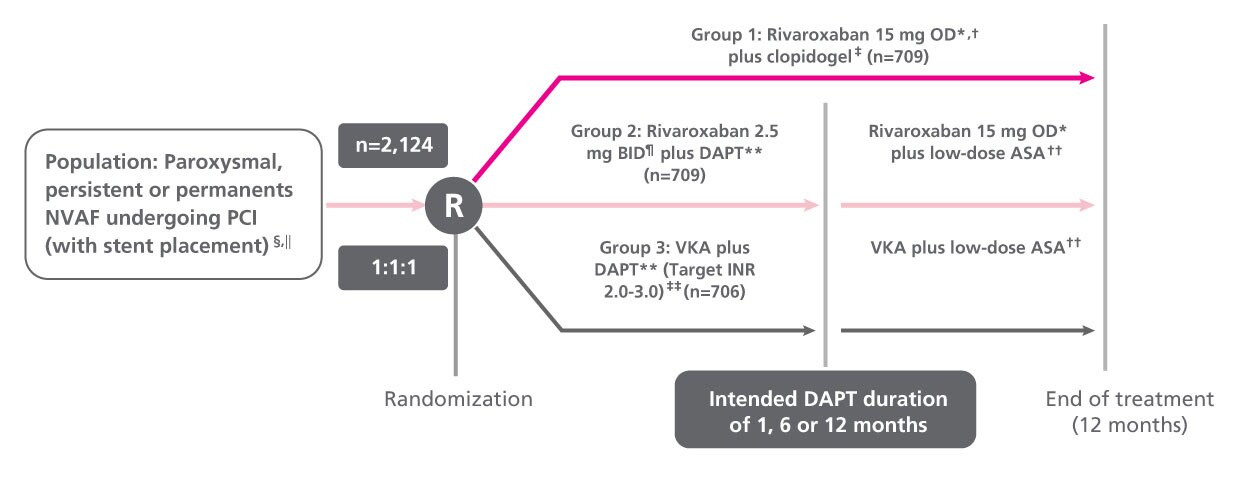
* Dose of rivaroxaban is reduced to 10 mg OD in subjects with CrCl 30 to 50 ml/min. † First dose 72 to 96 hours after sheath removal. ‡ Clopidogrel daily maintenance dose is 75 mg OD; alternate P2Y12 inhibitors: prasugrel 10 mg OD or ticagrelor 90 mg BID allowed (≤15% of participants). § NVAF is defined as AF not considered to be caused by a primary valve stenosis. ‖ Subjects with history of previous stroke or TIA were excluded. ¶ First dose 12 to 96 hours after sheath removal. ** DAPT consisted of low-dose ASA (75 to 100 mg OD) and P2Y12 inhibitor. †† ASA 75 to 100 mg OD. ‡‡ At the investigators discretion, an INR target of 2.0 to 2.5 may be used as some guidelines recommend.
Clinical End Points1
- Primary end point:
- The occurrence of clinically significant bleeding (a composite of major bleeding or minor bleeding according to TIMI criteria or bleeding requiring medical attention)
- Secondary end points:
- Incidence of each component of the primary safety end point
- Occurrence of a major adverse cardiovascular event (a composite of death from cardiovascular causes, MI or stroke)
- Each component of the major adverse cardiovascular event end point
- Rates of stent thrombosis
Key Findings
- Administration of either rivaroxaban 15 mg OD plus a P2Y12 inhibitor for 12 months or rivaroxaban 2.5 mg BID plus DAPT for 1, 6 or 12 months was associated with a lower rate of clinically significant bleeding vs standard therapy with a VKA plus DAPT for 1, 6 or 12 months1
- The rates for each component of the cardiovascular efficacy end point did not differ significantly among the three treatment groups1
AF , atrial fibrillation; ASA, acetylsalicylic acid; BID, twice daily; CrCl, creatinine clearance; DAPT, dual antiplatelet therapy; INR , international normalised ratio; MI , myocardial infarction; NVAF , non-valvular atrial fibrillation; OD, once daily; PCI, percutaneous coronary intervention; TIA , transient ischaemic attack; TIMI , thrombolysis in myocardial infarction; VKA , vitamin K antagonist.
PP-XAR-ALL-1817-1
References
- Gibson CM, et al. N Engl J Med. 2016;375:2423–2434. Gibson CM, et al. N Engl J Med. 2016;375:2423–2434. Return to content